Chapter 5: A TV producer with a breast lump
A 37-year-old TV documentary producer noticed a lump in her right breast whilst showering and was referred to the rapid access breast clinic for triple assessment (clinical, imaging, pathology). She is G1/P0 and has had two cycles of IVF a year ago. Her last menstrual period was 2 weeks ago. Her mother, maternal aunt and grandmother all had breast cancer. She is a non-smoker with a BMI of 30 and consumes 25 units of alcohol a week.
-
1. What factors influence her risk of breast cancer?
Show Answer
Correct answer:
- Family history (if >2 first-degree relatives are affected, the risk to other female family members doubles. There are four relatively common genes associated with an increased risk of breast cancer: BRCA1, BRCA2, CHEK2 and FGFR2)
- Duration of exposure to oestrogens (hence nulliparity, also early menarche, late menopause and hormone replacement therapy all increase risk)
- Diet (non-vegetarian diet, alcohol and coffee consumption and obesity increase the risk)
- Social class (women of social class I and II are at increased risk)
- Age (risk increases with age, plateauing around the menopause)
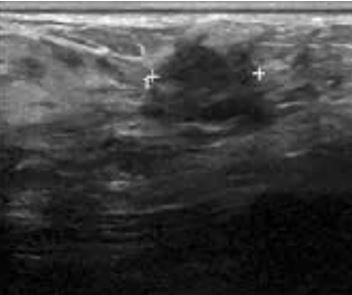
Breast ultrasound
-
2. What does the breast ultrasound show?
Show Answer
Correct answer:
There is a 6 cm mass palpable in the left outer quadrant (LOQ) of the right breast.
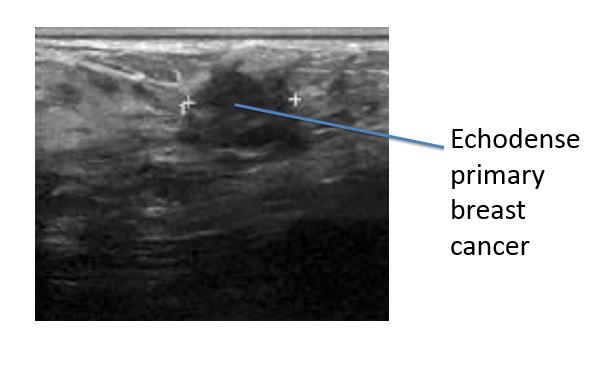
As she is <40 years old she has a breast ultrasound, core biopsy of the mass and fine needle aspirate (FNA) of the right axilla.
-
3. What clinical features of a breast lump make cancer more likely?
Show Answer
Correct answer:
- Hard
- Irregular
- Cold
- Non-tender
- No change during the menstrual cycle
- Nipple discharge or recent inversion
- Skin tethering or peau d’orange
- Presence of axillary lymph nodes
Of the breast cancers that are not detected by screening programmes, about 70% present as a painless lump, 5% as distortion of the breast including nipple inversion, 2% with a nipple discharge which is typically bloody and <2% present with isolated axillary lymphadenopathy whilst some patients present with features from metastatic spread such as bone pain, pleural effusions or hepatomegaly.
The FNA cytology is C5 (definitely malignant). FNA cytology is reported as: C1 (inadequate sample), C2 (definitely benign), C3 (probably benign), C4 (suspicious of malignancy) or C5 (definitely malignant).
The core biopsy shows invasive ductal carcinoma (IDC), grade 2 with extensive lymphovascular invasion (LVI). The Ki67 expression is 50% (this indicates high cell proliferation in breast cancer).
Immunohistochemistry (IHC) of the tumour was reported as:
- ER(oestrogen receptor) 6/8
- PgR(progesterone receptor) negative
- Her-2 3+.
IHC for ER is reported by the Allred system as a score 0-8 based on the percentage of cancer cells expressing ER on their surface and the intensity of expression. Her-2 IHC is reported as 0-1+ (negative), 2+ (borderline) and 3+ (positive). In borderline cases a second test, fluorescence in-situ hybridization (FISH) may be used to count the number of copies of the Her-2 gene per cancer cell.
-
4. What factors influence survival from breast cancer?
Show Answer
Correct answer:
- Tumour stage (primary tumour size, lymph node involvement and presence of metastases all influence prognosis)
- Tumour grade (several schemes are used by histopathologists to grade breast cancers, the Nottingham prognostic index combines T stage, N stage and tumour grade to predict 10-year survival in early breast cancer)
- Hormone receptor status (ER+ and PgR+ breast cancers have a better prognosis)
- Growth factor receptor status (a quarter of breast cancers express the epidermal growth factor receptor 2 (EGFR2), also known as Her-2/neu and c-erbB-2. Overexpression of Her-2 is associated with more aggressive behaviour and decreased disease-free survival)
- Age (women <35 years have double the risk of local recurrence and 1.6 times the risk of metastatic spread compared to older women >35 years)
- LVI(the presence of LVI is an independent risk factor for both local recurrence and metastatic spread)
She was offered neoadjuvant chemotherapy followed by wide local excision and axillary node clearance followed by adjuvant radiotherapy, trastuzumab and tamoxifen. Naturally she wanted to make a video diary of her experiences for broadcasting on Channel 4.
-
5. What are the options for fertility conservation?
Show Answer
Correct answer:
- *Egg harvesting (at present ovum storage remains an unreliable method for routine usage and requires ovarian stimulation prior to egg harvesting, which introduces a delay prior to starting chemotherapy and is relatively contraindicated in breast cancer)
- *Ovarian strip cryopreservation (experimental strategy that attempts to harvest ova without ovarian hyperstimulation and the delay that it entails)
- *Ovarian suppression (use of gonadotropin-releasing hormone (GnRH) suppression during chemotherapy has been used in an attempt to reduce oocyte damage)
- Storage of fertilized ova (storage of embryos is the most reliable method of conserving fertility in women)
- Egg donation (donor eggs fertilized by chosen sperm and implanted into the uterus)
- Embryo donation (donor embryos implanted into the uterus)
*currently viewed as experimental
-
6. What are the three most common psychological effects in breast cancer survivors?
Show Answer
Correct answer:
- The Lazarus syndrome (difficulty returning to normal mundane life)
- The Damocles syndrome (fear of cancer recurrence and terror of even trivial symptoms)
- The Survivor syndrome (guilt about surviving cancer where others have died)